What is Minimally Invasive Spine Surgery?
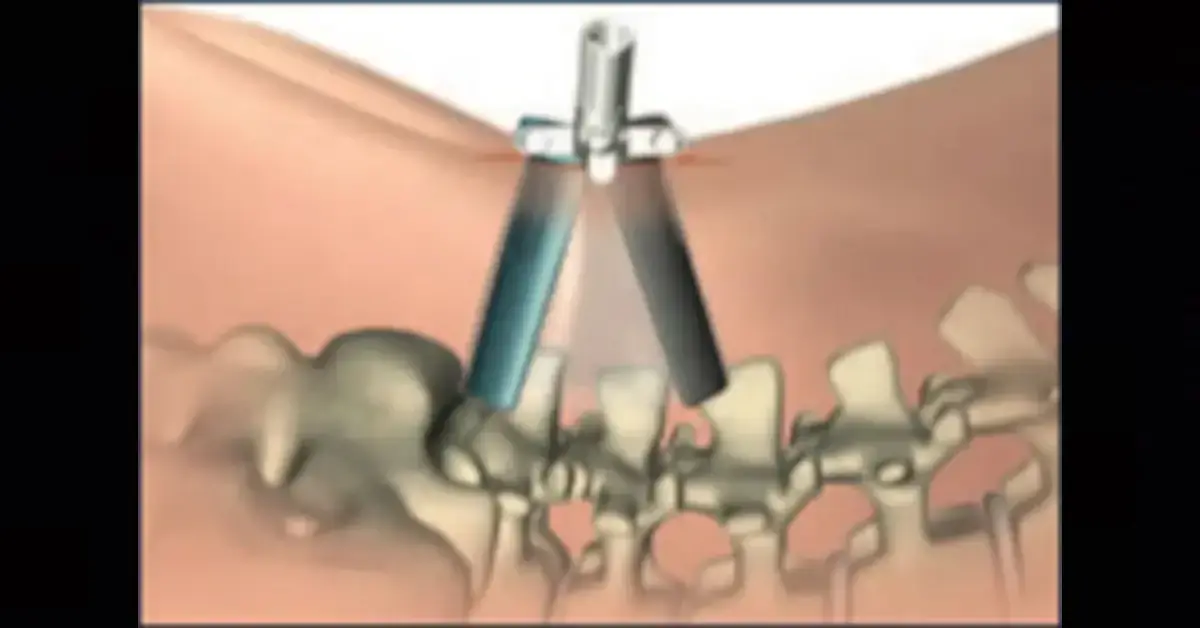
Minimally Invasive Spine Surgery (MIS) is a general term used to describe a variety of surgical techniques which involve making smaller incisions and reducing the amount of tissue damage beneath the skin. In spinal surgery, minimally invasive surgery is accomplished with the aid of specially designed instruments which assist in visualization of the surgical field. Typically, this is done with tubular retractors such as Luxor™ which allows the surgeon to make a small incision but visualize a larger area beneath the small incision. Spine surgeons who perform minimally invasive spine surgery should be fully trained in the correct use of these techniques.
What is the future of Minimally Invasive Spine Surgery?
Newer areas for minimally invasive techniques include the fusion of two vertebrae together and expanding endoscopic procedures (meaning: the surgery is performed through little holes in the skin as opposed to a larger incision). The field of minimally invasive spine surgery is growing rapidly and the overall trend is toward more minimally invasive techniques and new procedures. New instruments and techniques such as Stryker’s Luxor™ and Techtonix™ systems are being well received by the market.
What are the potential benefits of Minimally Invasive Spine Surgery?
The potential benefits of minimally invasive spine surgery may include smaller scars following the operation and less damage to the surrounding tissues beneath the skin, meaning less pain and blood loss. The potential outcomes of such operations are the reduction of pain and morbidity associated with standard open surgery. At the moment there is insufficient data to show that minimally invasive spine surgery provides any short and long term benefit to patients when compared to traditional spine surgery.
Is everyone suitable for MIS surgery?
No. There are many factors to consider including age, weight, lifestyle and procedure required. This must all be discussed with your spine surgeon. Typically the following groups of people are not candidates for Minimally Invasive Surgery:
- Unstable medical conditions that may lead to a higher risk of complications
- Prior spine surgery in the same location What should I do to prepare for surgery?
Your doctor will perform a clinical examination and possibly a few tests prior to surgery to see if you are a candidate for the procedure. These may include an MRI, discography, CT scan and X-rays. Tell your surgeon what medications you are taking and ask if you should stop taking them before your operation. If you smoke, stop smoking as this slows the ability of bone to grow and repair adequately.
To make your recovery easier, prepare your home for life after surgery. Arrange for someone to help you at home after surgery. You’ll most likely be told not to eat or drink the night before the surgery.
What can I typically expect after surgery?
After the operation, you may experience pain at the site of the surgery. Your surgeon may prescribe pain or anti-inflammatory medication. Take it as directed.
You will normally go through a postoperative care program with instructions to help you recover from the surgery. It is extremely important that you follow the rehabilitation guidelines given to you by your surgeon.
How can I learn more?
Your spine surgeon will be happy to answer any additional questions you may have.
For more information, please visit the following websites:
Patient Checklist
Before Surgery
- Stop smoking
- Remove hazards at home and put items within reach
- Stop taking aspirin and ibuprofen (or any non-steroidal anti-inflamatory drugs) several days before surgery
- Don’t eat or drink after midnight prior to surgery
After Surgery
- Take your pain medication as directed
- Follow physical rehabilitation plan as prescribed
- Do not drive until your surgeon approves
- Schedule your post-operative exam
Long-Term Recovery
- Ask your surgeon about resuming work and other activities
- Attend follow-up exams following your rehabilitation program as recommended by your surgeon
When should I call my surgeon?
You should call your surgeon if you notice any of the following:
- Increased back or leg pain, numbness, tingling or weakness that does not decrease with rest
- Swelling in your legs
- Increased pain, redness or drainage from your incision
- Fever
- Chest pain
* Always follow the instructions from your physician